What is Pelvic Organ Prolapse?
What is the pelvic organ?
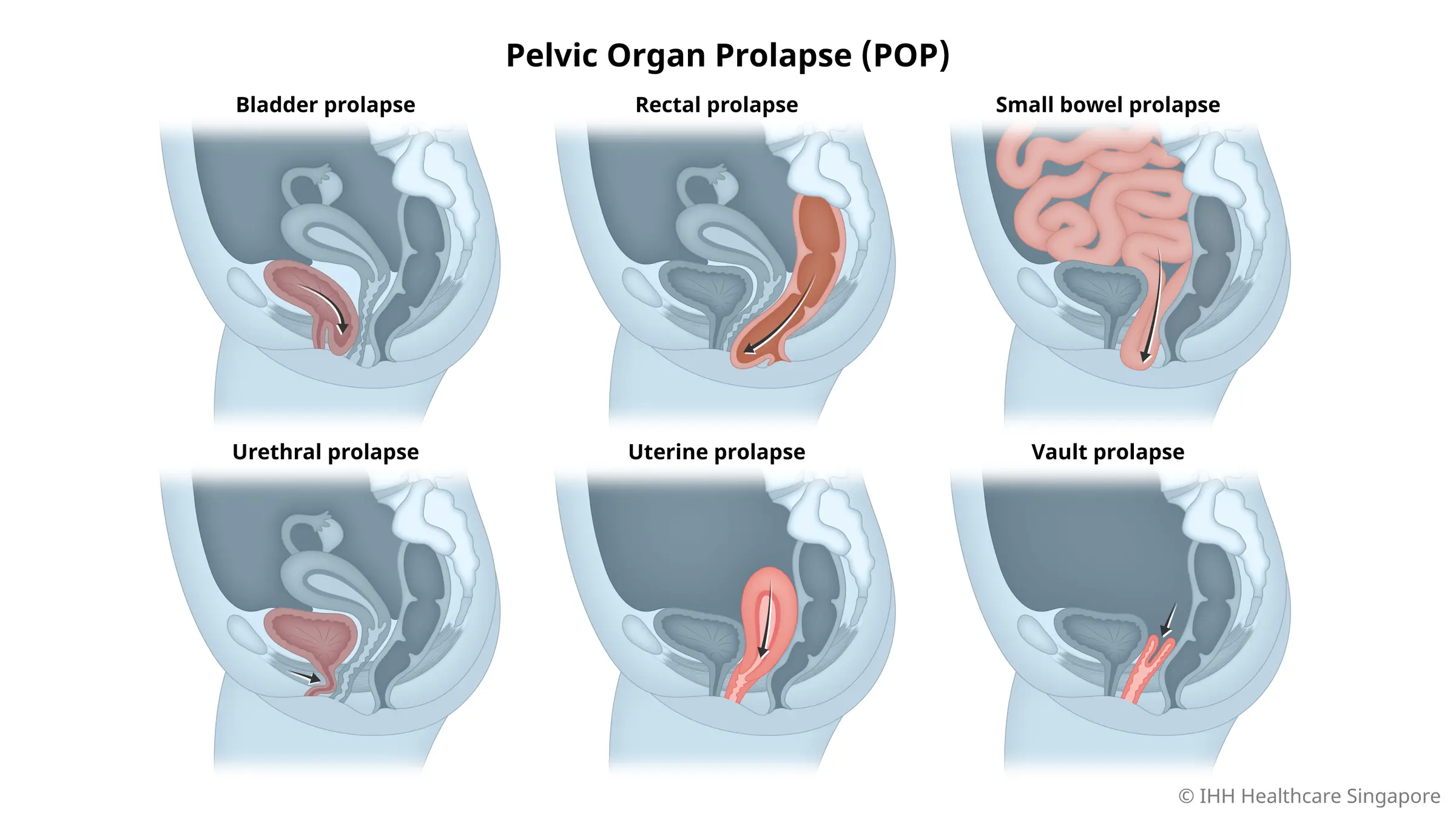
What are the types of pelvic organ prolapse?
Pelvic organ prolapse involves the descent of pelvic organs, and it can manifest in several distinct types, each affecting the body differently. Understanding these types is crucial for recognising symptoms and seeking appropriate treatment. Here are the primary types of pelvic organ prolapse:
This type occurs when the bladder drops from its normal position and bulges into the front wall of the vagina. It typically results from weakened pelvic floor tissues, often due to childbirth or chronic straining. Common symptoms include a feeling of fullness in the vagina, urinary incontinence, frequent urination, and difficulty emptying the bladder completely.
An enterocele involves the small intestine descending into the pelvic cavity, creating a bulge in the vaginal wall. It often occurs after a hysterectomy and can lead to symptoms such as pelvic pressure, backache, and a feeling of vaginal fullness.
This occurs when the uterus slips down into the vaginal canal due to weakened pelvic support structures. Symptoms often include a sensation of heaviness or pulling in the pelvis, tissue protruding from the vagina, and lower back pain. It may also cause urinary and sexual dysfunction.
- Grade 1 (Mild Prolapse): The slightly descends into the vagina but remains above the opening. Symptoms are usually minimal or absent.
- Grade 2 (Moderate Prolapse): The uterus descends closer to the vaginal opening but does not protrude. Symptoms like pelvic pressure and mild urinary issues may appear.
- Grade 3 (Advanced Prolapse): The uterus protrudes slightly outside the vaginal opening, causing noticeable discomfort, pelvic pressure, and urinary or bowel difficulties.
- Grade 4 (Severe Prolapse, Procidentia): The entire uterus protrudes outside the vaginal opening, leading to severe symptoms and significant impact on daily life.
Symptoms of Pelvic Organ Prolapse
Pelvic organ prolapse can manifest through several impactful symptoms that may affect daily activities and overall well-being. Here are the most common symptoms to be aware of:
A constant feeling of heaviness or pressure in the pelvic area, often worsening as the day progresses.
Noticeable bulging tissue at the vaginal opening, which can be seen or felt.
- Challenges such as urinary incontinence (leakage) or retention (difficulty fully emptying the bladder).
Issues with bowel movements, including straining or constipation.
Pain or discomfort during sexual activity, which can impact intimacy and emotional health.
Persistent pain in the lower back that may increase throughout the day.
If you experience these symptoms, it’s crucial to seek advice from a healthcare professional for an accurate diagnosis and appropriate treatment options. Addressing these symptoms early can help improve quality of life and manage the condition effectively.
Causes of Pelvic Organ Prolapse
Pelvic organ prolapse occurs when the muscles and tissues that support the pelvic organs become weak or damaged. This can be caused by a variety of factors, including:
- Pregnancy and Childbirth: The physical demands of carrying and delivering a baby can weaken the pelvic floor.
- Menopause: Hormonal shifts during menopause can further diminish pelvic floor strength.
- Obesity: Extra body weight increases pressure on pelvic organs, heightening prolapse risk.
- Chronic Coughing: Persistent coughing exerts strain on pelvic muscles, leading to potential weakening.
- Genetic Factors: A hereditary predisposition can make some individuals more susceptible to prolapse.
Complications of Pelvic Organ Prolapse
Pelvic organ prolapse can lead to various complications that may affect different aspects of life. Here are some potential complications to be aware of:
- Urinary Incontinence: Difficulty controlling urination, leading to involuntary leakage, is common among those with prolapse.
- Bowel Dysfunction: Challenges with bowel movements, such as constipation or faecal incontinence, can arise.
- Sexual Dysfunction: Pain or discomfort during intercourse may impact sexual health and relationships.
- Recurrent Urinary Tract Infections: Increased risk of urinary tract infections due to changes in urinary function.
- Emotional or Psychological Impacts: The symptoms and complications of prolapse can lead to stress, anxiety, or depression, affecting overall well-being.
It’s vital to consult a healthcare professional for appropriate management and treatment options to address these complications and improve quality of life.
Diagnosis of Pelvic Organ Prolapse
Diagnosing pelvic organ prolapse is a comprehensive process that involves several essential steps, all guided by a healthcare professional. Here’s a closer look at what to expect during this evaluation:
- Physical Examination: Our urogynaecologist investigates any signs of prolapse and evaluates the strength and integrity of the pelvic floor muscles.
- Detailed Medical History: Discussing any past pregnancies, surgeries, or symptoms you’ve experienced, which helps our urogynaecologist identify underlying causes and contributing factors.
- Symptom Evaluation: Our urogynaecologist will inquire about issues such as urinary difficulties, lower back pain, or pelvic discomfort to assess the severity and impact on daily life.
- Advanced Imaging Tests: If necessary, imaging tests like ultrasound or MRI may be utilised to gain a more precise view of the pelvic organs. These tests offer detailed insights into the extent of the prolapse, aiding in the development of a tailored treatment plan.
Consulting with our urogynaecologist is vital for obtaining an accurate diagnosis and effective treatment plan. Early and precise diagnosis can lead to better management strategies and significantly enhance quality of life.
How is Pelvic Organ Prolapse Treated
The treatment approach for POP depends on its type and severity. In Singapore, doctors may recommend non-surgical options such as:
- Pelvic floor muscle exercises: Also known as Kegel exercises, these can help strengthen the pelvic floor muscles and improve support for the pelvic organs.
- Lifestyle modifications: Maintaining a healthy weight, avoiding constipation, and quitting smoking can also help reduce symptoms of POP.
- Use of pessaries: These are removable devices that can be inserted into the vagina to support the pelvic organs and alleviate symptoms.
In severe cases or when non-surgical options do not provide relief, surgery may be recommended. The type of surgery will depend on the specific organ affected and the patient’s overall health. It is essential to discuss all options with your doctor and understand the benefits and risks of each before making a decision.
After treatment, it is crucial to take steps to manage symptoms and prevent recurrence. This may include maintaining a healthy lifestyle, continuing pelvic floor muscle exercises, and regular follow-up with your doctor.
Prevention of Pelvic Organ Prolapse
While there is no guaranteed way to prevent pelvic organ prolapse, there are steps that women can take to lower their risk. These include:
Excess weight puts added strain on the pelvic organs, making them more vulnerable to prolapse.
Strengthening the pelvic floor muscles can help prevent or delay prolapse.
These activities can put pressure on the pelvic floor and increase the risk of prolapse.
If left untreated, these conditions can weaken the pelvic floor muscles and contribute to prolapse.
Disclaimer: The information provided in this article is for general purposes only and should not be considered as a substitute for medical advice. Always consult with your healthcare provider before making any changes to your current treatment plan or starting any new medications.
